Recall 1:
Q- Directly Observed Therapy (DOT) in Tuberculosis (TB)?
Right is: 3 times per week✔️
DOT = Directly Observed Therapy، وهو نظام علاج لمرض السل (TB) يتم فيه إعطاء الدواء للمريض تحت الملاحظة المباشرة من مقدم الرعاية الصحية، لضمان أنه أخذ الجرعة فعلاً.
🔹 يعني أن المريض المصاب بالسل يأخذ العلاج 3 مرات في الأسبوع وتحت الإشراف المباشر من قبل Directly Observed Therapy.
Recall 2:
Q- Which of the following is more specific for tuberculosis (TB)?
A. Pyrexia
B. Bilateral hilar lymphadenopathy
Note حجازي:
In conclusion, while pyrexia is a common symptom of TB, bilateral hilar lymphadenopathy is a more specific radiological finding associated with TB, making it the more specific indicator of the disease between the two options provided.
Recall 3:
Q- What is the first symptom to appear in tuberculosis (TB)?
A. Pyrexia
B. Lymphadenopathy
C. Sweating
D. Weight loss
Correct answer: A. Pyrexia ✔️
Recall 4:
Q- Which of the following radiological features is characteristic of miliary tuberculosis?
A. Sparing of the lung apices❌
B. Pleural effusion❌
C. Septal lines❌
D. Absence of glandular enlargement❌
E. Presence of a small cavity
احتمال يكون هذا لكن الإجابة مو دقيقة
مفروض الإجابة الصحيحة تكون حسب كلام حجازي:
Presence of multiple tiny nodules (1–3 mm) diffusely and uniformly distributed throughout both lungs
Recall 6:
Q- When should the response to tuberculosis (TB) treatment be checked?
A. 1 month
B. 2 months
C. 3 months
D. 4 months
Right is: B. 2 months
Recall 7:
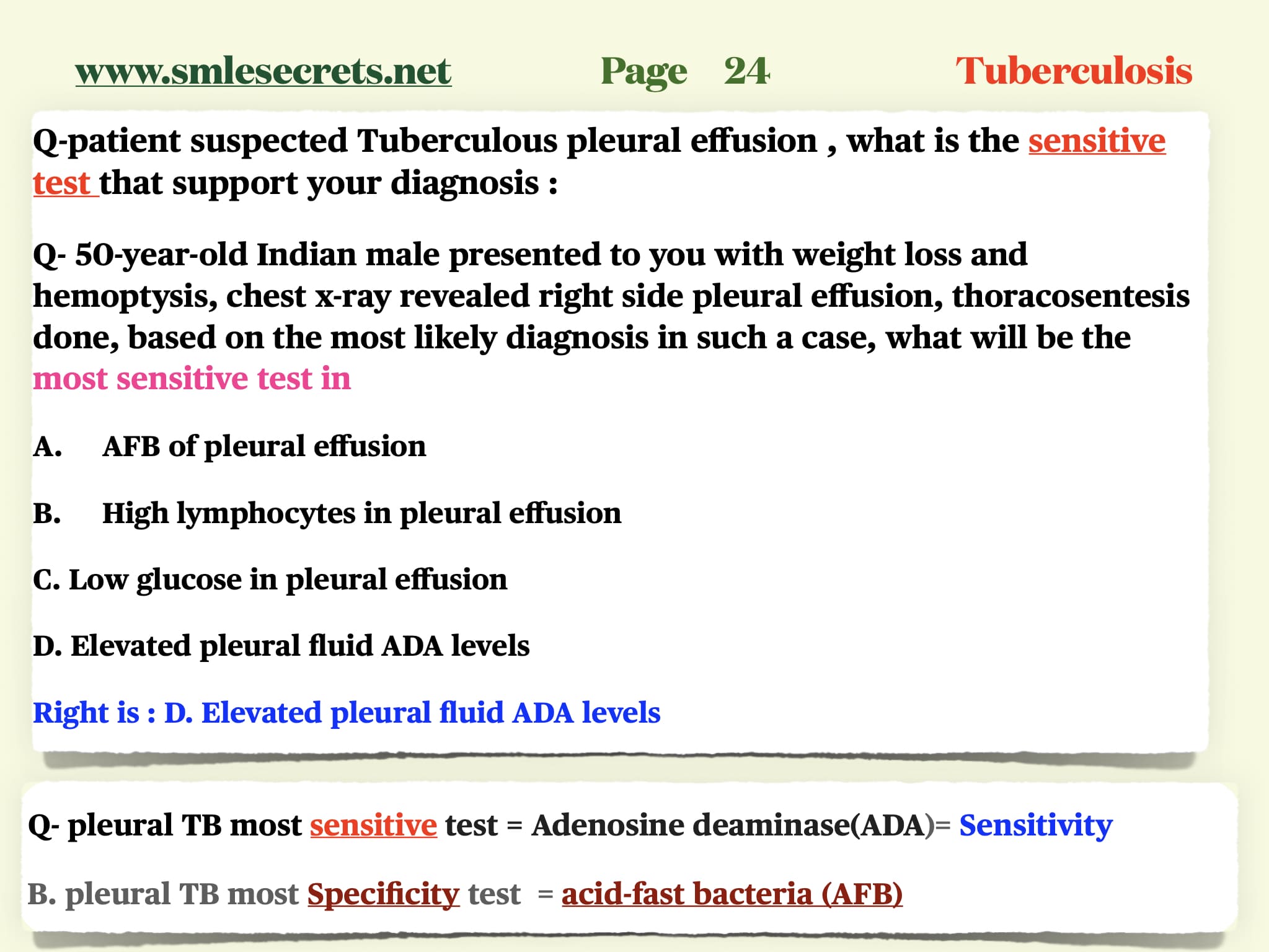
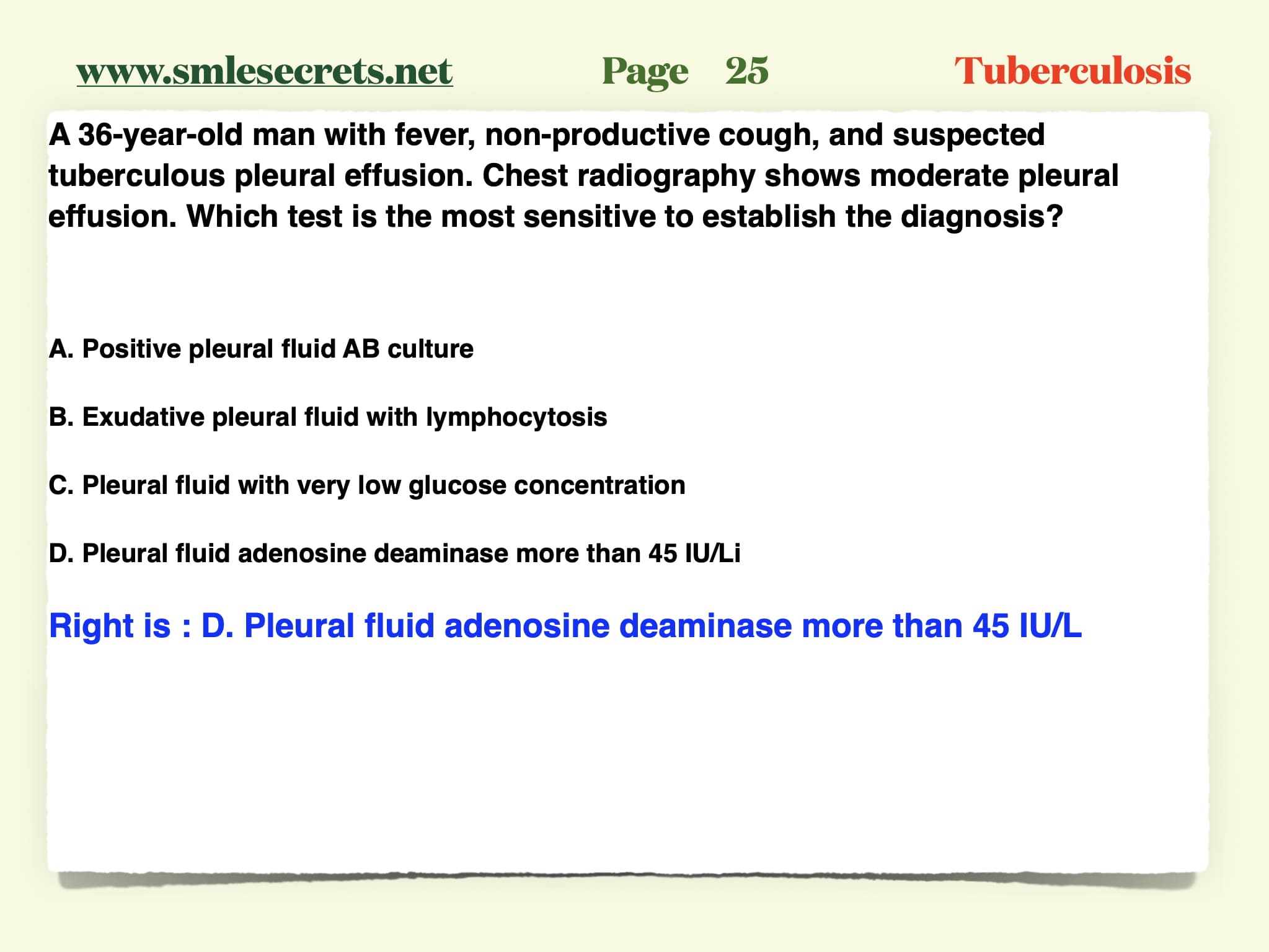
Q- Old patient with fever/weight loss/ lethargy and chest X-ray showed pleural effusion. They did thoracentesis with sampling and found interferon gamma?
A. Mesothelioma
B. Tuberculous (TB)
Right is: Tuberculous (TB)
Note: Interferon gamma is indicative of tuberculous pleural effusions
Recall 8:
Q- Pleural effusion case and has high interferon gamma. Diagnosis?
A. Pleural tuberculosis
B. Pneumonia
C. Lung cancer
D. ILD (Interstitial Lung Disease)
Right is: Pleural tuberculosis
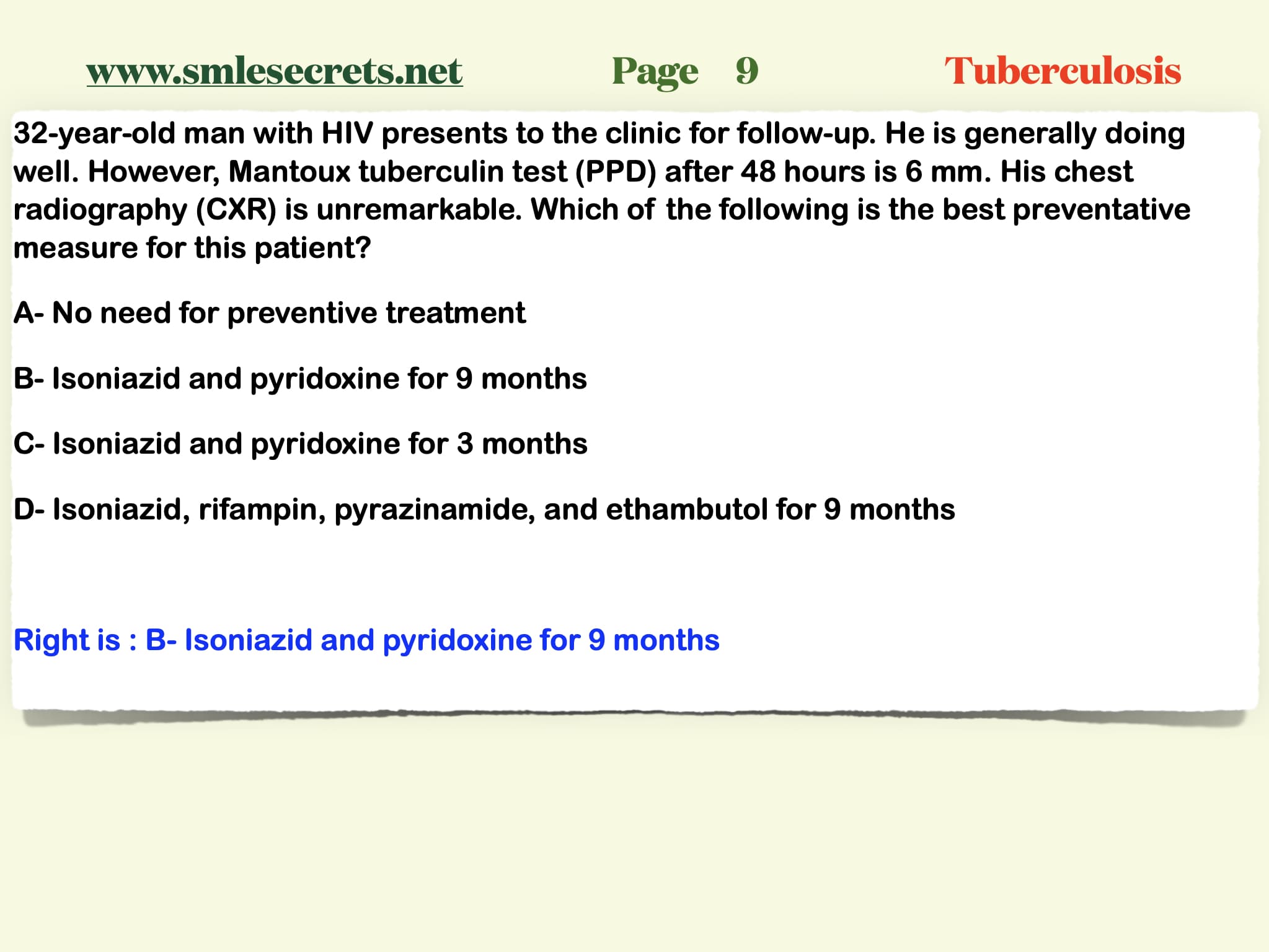
Recall 9:
Q- Patient with TB. CXR revealed pleural effusion. How to know the effusion is due to TB?
A. Pleural protein over serum is < 0.3
B. Pleural LDH > 100
C. Pleural WBC > 1000
D. Pleural LDH over serum > 1/3
Right is: Pleural WBC > 1000
Recall 10:
Q- Patient with TB, chest X-ray revealed pleural effusion. How to know the effusion is due to TB?
A. LDH more than upper 1/3 of normal
B. LDH more than upper 2/3 of normal
C. Pleural:Serum Protein < 0.5
D. Pleural:Serum LDH < 0.6
Right is: B. LDH more than upper 2/3 of normal
right is : B. Plural pLDH/ serum LDH is MORE than 0.6
Recall 11:
Q- Middle age male complains of SOB, CXR evidence of pleural effusion. Aspiration of fluid to analysis was done. What statement of the following confirm that the pleural effusion is exudative?
A. Plural protein/serum protein is LESS than 0.5
B. Plural pLDH/ serum LDH is MORE than 0.6
C. LDH is more the 1/3 of upper limit ..
right is : B. Plural pLDH/ serum LDH is MORE than 0.6
Recall 12:
Q- most likely cause of bilaterally calcified adrenal glands in a patient with Addison’s disease?
A. Autoimmune adrenalitis
B. Tuberculosis
B. Tuberculosis
Note :
-
Tuberculosis is a classic cause of bilateral adrenal calcification leading to Addison’s disease (primary adrenal insufficiency), especially in countries where TB is still prevalent.
-
Autoimmune adrenalitis is the most common cause of Addison’s in developed countries, but does not usually cause calcification.
-
Metastasis and fungal infections may affect the adrenals, but calcification bilaterally is more specific to chronic TB.
Recall 13:
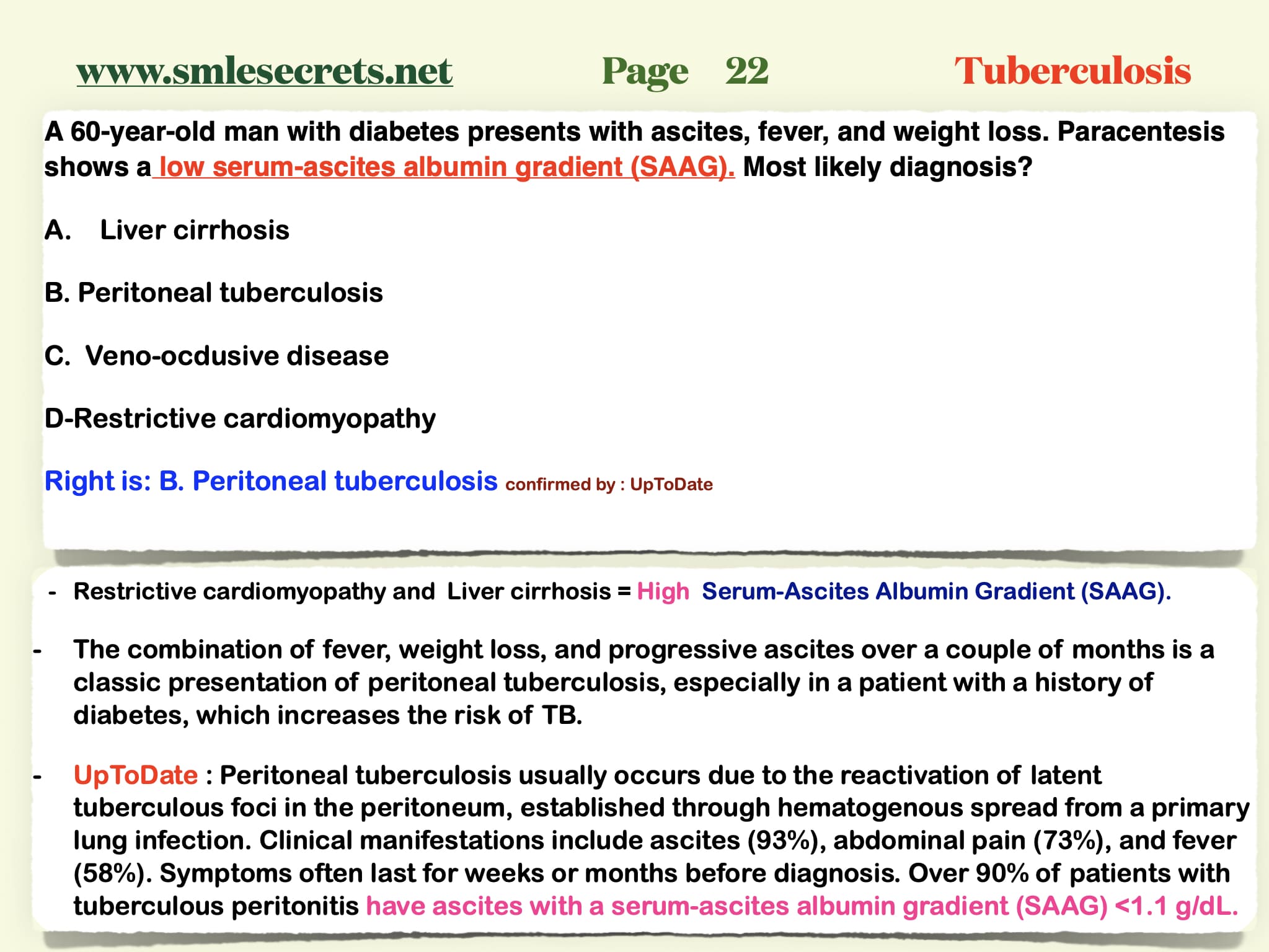
A patient presents with fever, ascites, and a serum-ascites albumin gradient (SAAG) less than 1.1 g/dL. What is the most likely diagnosis?
A. Cirrhotic ascites
B. Malignant ascites
C. Tuberculous peritonitis
D. Congestive heart failure
Right is : C. Tuberculous peritonitis
Recall 14:
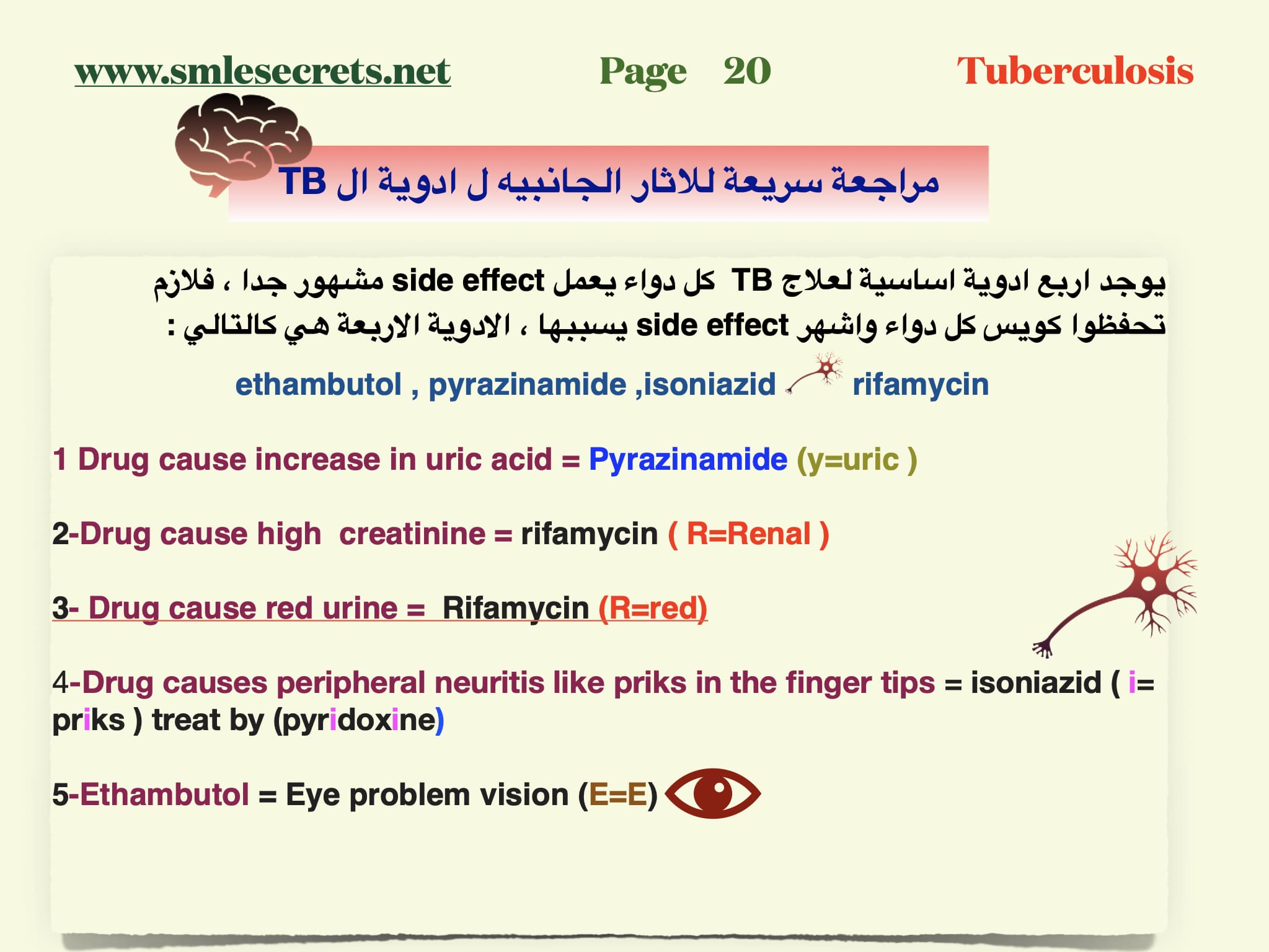
Which anti-tuberculosis drug is associated with hyperuricemia and arthritis (especially gout)?
A. Isoniazid
B. Rifampicin
C. Ethambutol
D. Pyrazinamide ✅
Recall 15:
A patient on anti-TB treatment develops arthritis with swelling and pain in the big toe. Which drug is most likely responsible?
A. Isoniazid
B. Rifampicin
C. Pyrazinamide ✅
D. Streptomycin
Recall 16:
Which TB drug can cause gout as a side effect due to increased uric acid levels?
A. Ethambutol
B. Rifampicin
C. Pyrazinamide ✅
D. Isoniazid
Recall 17:
A patient receiving anti-tuberculosis therapy presents with isolated hyperbilirubinemia. Which drug is the most likely cause?
A. Ethambutol
B. Rifampicin
C. Pyrazinamide ✅
D. Streptomycin
Recall 18:
A patient with congestive heart failure (CHF) and hypertension (HTN) is on ACE inhibitors and warfarin. He is newly diagnosed with tuberculosis and started on anti-TB therapy including rifampicin.
What adjustment should be made and why?
A. Stop ACE inhibitor to avoid interaction
B. Reduce warfarin dose due to bleeding risk
C. Increase warfarin dose as rifampicin decreases its effect ✅
D. No change needed in warfarin dose
Recall 19:
A patient with a history of pulmonary tuberculosis develops bronchiectasis and later is found to have pulmonary hypertension.
What is the most likely underlying cause of the pulmonary hypertension?
A. Active TB infection
B. Pulmonary embolism
C. Pulmonary fibrosis ✅
D. Right heart failure
Recall 20:
Which anti-tuberculosis drug is most likely to cause a maculopapular rash?
A. Isoniazid (INH) ✅
B. Pyrazinamide
C. Ethambutol
D. Streptomycin
Recall 21:
A 45-year-old man on n isoniazid, rifampin, pyrazinamide and ethambutol therapy has AST 75 IU/L (normal < 40), normal bilirubin, and feels well. Sputum AFB is negative. What’s the best next step?o. He came back to the clinic for follow up after 3-weeks Cough was better and no other symptoms (see lab results) Total bilirubin 5 3 5-16.5 pmol/L Which of the following is the best management approach?
A. Continue anti-TB and repeat LFT in 1 week
B. Stop all anti-TB and repeat LFT in 1 weeks
C. Stop pyrazinamide and repeat LFT in 2 weeks
D. Stop isoniazid and rifampin and repeal LFT in 2 weeks
Right is : A. Continue anti-TB and repeat LFT in 1 week
Recall 22:
A patient is receiving anti-tuberculous therapy and after three weeks, liver function tests (LFTs) show elevated transaminases.
What is the most appropriate next step in management?
A. Continue all drugs and monitor
B. Stop only INH
C. Stop all anti-TB drugs ✅
D. Replace Rifampicin with another drug
Recall 23:
A patient with end-stage renal disease and an estimated glomerular filtration rate (eGFR) of 15 mL/min is being treated for tuberculosis.
How should the dosing of Ethambutol be adjusted?
A. Daily dosing as usual
B. Reduce dose to half daily
C. Administer every 48 hours (( 3 times/ wk ))
D. Stop Ethambutol completely
-
Ethambutol يتم إخراجه بشكل رئيسي عن طريق الكلى، ولذلك في حالات القصور الكلوي (مثل eGFR ≤ 30 mL/min) يجب تعديل الجرعة.
-
في المرضى الذين يعانون من eGFR 15 (يعني قصور كلوي شديد أو مرحلة ما قبل الغسيل)، يُوصى بـ:
-
إعطاء الجرعة المعتادة لكن كل 48 ساعة، أو 3 مرات في الأسبوع.
-
وذلك لتفادي تراكم الدواء وحدوث سمية بصرية (optic neuritis
-
Recall 24:
Q- mother with TB cangive breastfeeding to her son?
A-directbreastfeedingHIVmother
B-expressed milk HIV mother
C-directbreastfeedingTB mother
D-expressedmilkTBmother
Right is : expressedmilkTBmother
Recall 25:
Q- the primary prevention for tuberculosis (TB)?
right is vaccination ✅
Recall 26:
restrictive lung disease predisposes to tuberculosis (TB)?
A. Asthma
B. Pulmonary fibrosis
C. Silicosis ✅
D. Chronic obstructive pulmonary disease (COPD)
Recall 27:
A patient with a history of tuberculosis (TB) 10 years ago presents with cough and hemoptysis, Patient In Consultation, A chest X-ray shows an apical lesion. What is the most likely diagnosis?
A. Pneumonia
B. Mycetoma ✅
right is “: Myocytoma
Recall 28:
A patient who was treated for tuberculosis (TB) 3 years ago presents with shortness of breath (SOB), hemoptysis, and fever. A chest X-ray shows an apical lesion.
What is the most likely diagnosis?
A. Pneumonia
B. Reactivation of TB ✅
C. Lung cancer
D. Mycetoma
Recall 29:
When diagnosing a patient with tuberculosis (TB), what is the first step in management?
A. Start anti-TB medication immediately
B. Isolate the patient in a negative pressure room and perform liver function tests (LFTs) before starting medication ✅
C. Start corticosteroids
D. Perform a sputum smear and start treatment after 24 hours
Recall 30:
A patient with tuberculosis (TB) is found to be resistant to both Rifampicin and Isoniazid (INH). What is the next best step in management?
A. Continue the 4-drug regimen for 6 months
B. Stop Rifampicin and INH, and give Amikacin + Levofloxacin
C. Increase the dose of INH
D. Add corticosteroids
Right is : B. Stop Rifampicin and INH, and give Amikacin + Levofloxacin ✅
Recall 31:
A patient with tuberculosis (TB) is found, after 8 weeks of standard 4-drug therapy, to have resistance to both Isoniazid (INH) and Rifampicin. What is the next best step in management?
A. Continue the same 4 drugs for one year
B. Replace INH and Rifampicin with two other drugs and continue the remaining 3 drugs
C. Stop all current drugs and give only Ciprofloxacin and Doxycycline
right is : B. Replace INH and Rifampicin with two other drugs and continue the remaining 3 drugs ✅
Recall 32:
A patient presents with severe pulmonary tuberculosis. What is the best initial drug combination to start treatment?
A. INH + Rifampicin + Ethambutol + Pyrazinamide ✅
B. INH + Rifampicin + Streptomycin
C. INH + Rifampicin + Ciprofloxacin
…
Recall 33:
Gamma interferon release assays (IGRAs) are primarily used for which of the following purposes?
A. Mantoux test
B. Latent tuberculosis ✅
C. Active tuberculosis
D. Monitor response to treatment
Recall 34:
What is the recommended frequency for Directly Observed Therapy (DOT) in tuberculosis treatment?
A. Daily
B. Three times per week ✅
C. Once weekly
D. Only during the intensive phase
Recall 35:
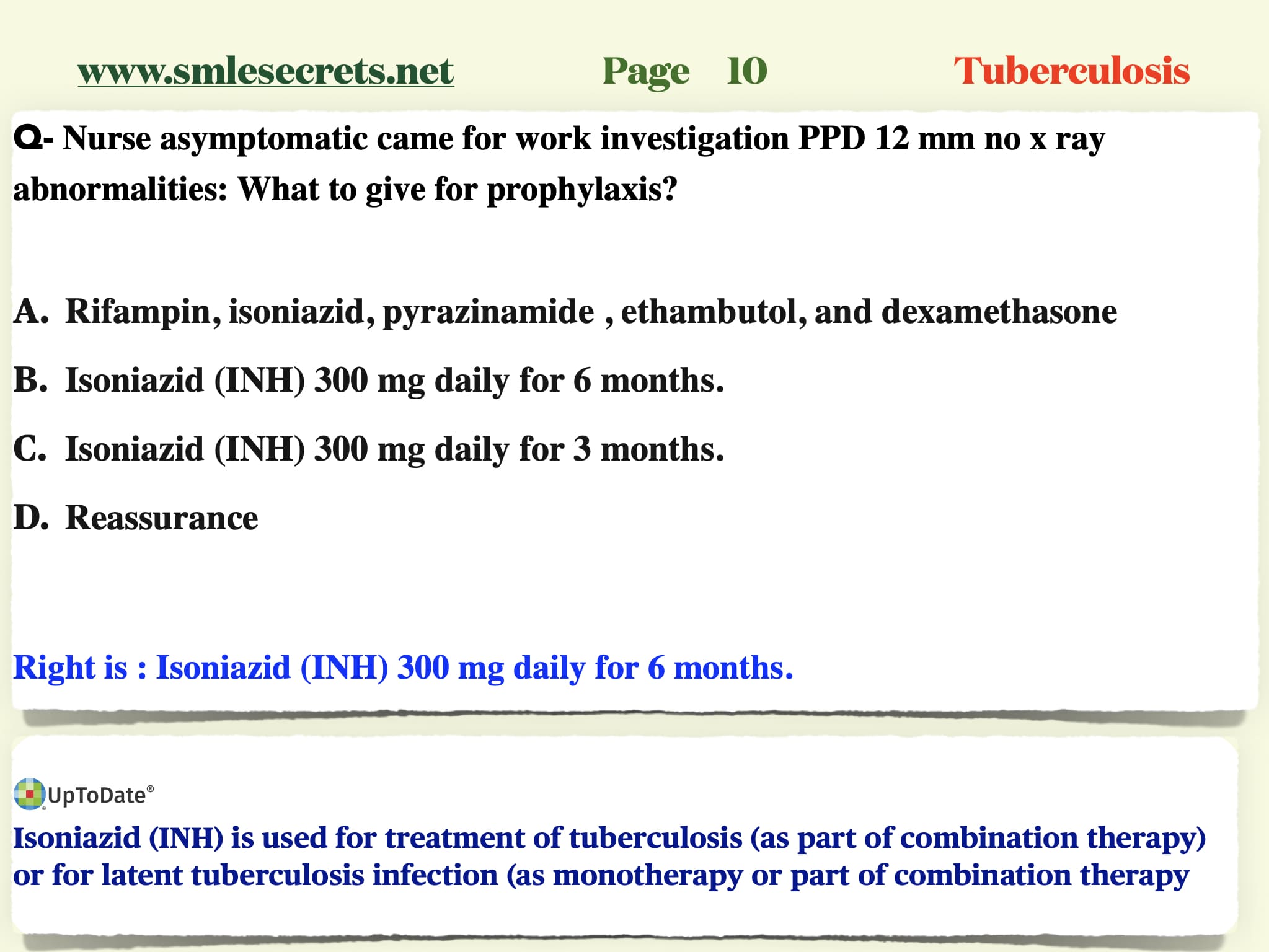
A patient had contact with a TB case, has no symptoms, normal chest X-ray, but a tuberculin skin test (TST) of 15 mm. What is the next best step?
A. Reassure and observe
B. Start Isoniazid (INH) for 6 months ✅
Recall 35:
What is the recommended prophylaxis for TB after contact with an active case?
A. Isoniazid (INH) for 6 months
B. INH + Rifampicin for 3 months ✅
Recall 36:
A patient presents with signs of meningitis. CSF analysis shows low glucose, and a CT brain reveals a ring-enhancing lesion. What is the most likely diagnosis?
A. Bacterial meningitis
B. Neurocysticercosis
C. Toxoplasmosis
D. Tuberculous meningitis ✅
Recall 37:
picture shows ash leaf spots and facial angiofibromas. What is the most likely diagnosis?
A. Neurofibromatosis
B. Tuberous Sclerosis ✅
Recall 38:
A TB patient presents with pigmentation, hypotension, shock, and hyponatremia. What is the most appropriate treatment?
A. Short-term sodium supplementation
B. Long-term sodium supplementation
C. Short-term corticosteroids
D. Long-term corticosteroids✅
Recall 39:
A patient presents with a hypopigmented area and decreased sensation. What is the most likely diagnosis?
A. Lepromatous leprosy
B. TB Leprosy ✅
Recall 40:
A patient with a history of previous pulmonary tuberculosis treated, IV drug abuse, and presenting with fever, rigor, cough, pansystolic murmurs (tricuspid regurgitation), and hepatomegaly. What is the most likely diagnosis?
A. Infective endocarditis with septic emboli ✅
B. Recurrent TB
C. Bronchiectasis
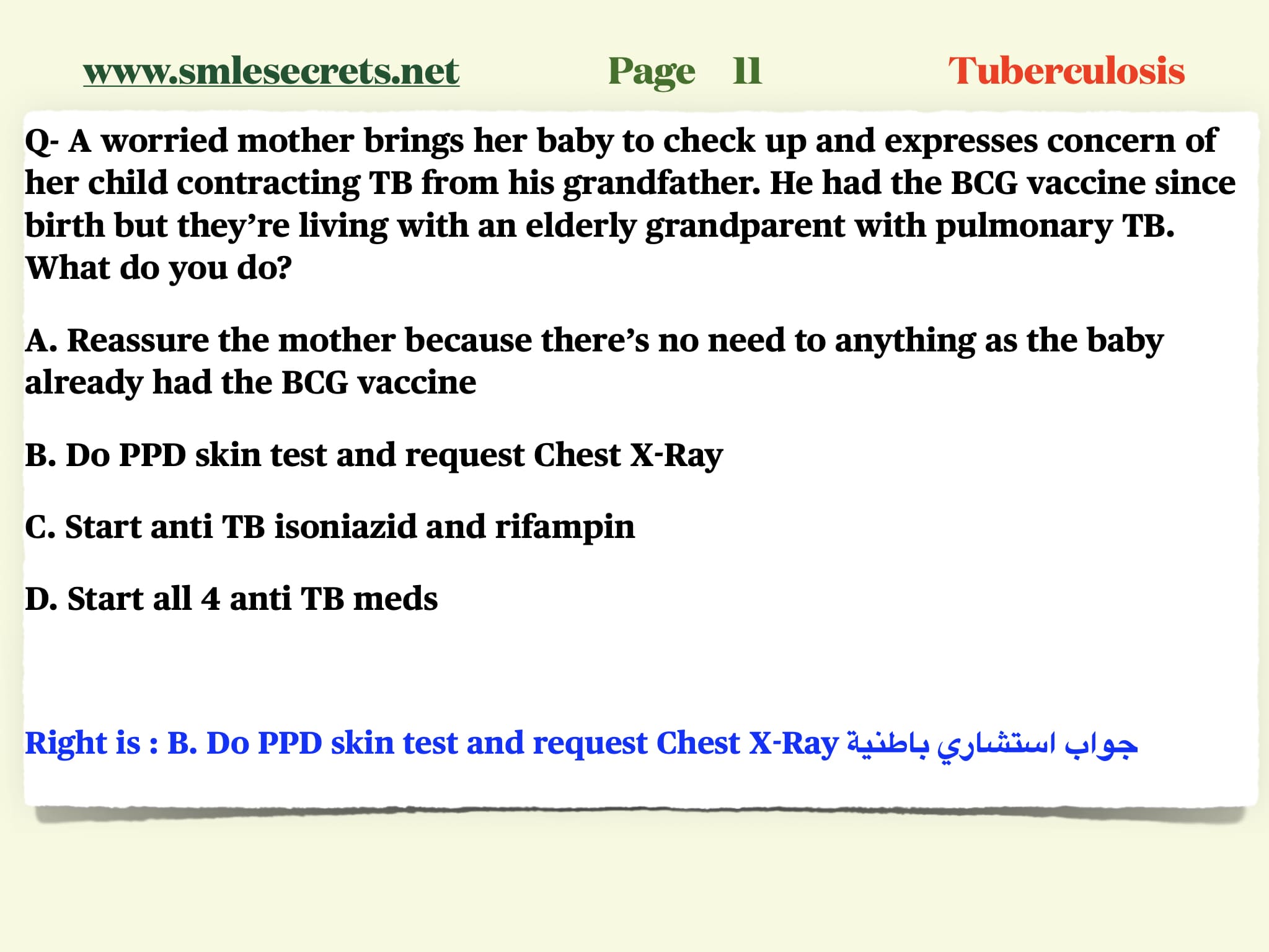
Recall 41 :
A 40-year-old female who had BCG vaccination at birth and has contact with her grandmother who is TB positive. What is the next step?
A. CXR
B. Tuberculin Test ✅
تجميعات من طب عام اختبار الهيئة السعودي ممكن يجي نفس الاسئلة